In medicine motility is often spoken of as movement; food moves forward the stomach empties or the transit is delayed or accelerated. This way of nomenclature is simple, measurable, and deeply misleading.
Motility is a coordinated process that depends on timing, rhythm, sequencing, and feedback. When we reduce it to movement alone, we miss the essence of how the gut actually functions.
Nowhere is this misunderstanding more consequential than in disorders where symptoms are real, tests are normal, and explanations remain unsatisfying.
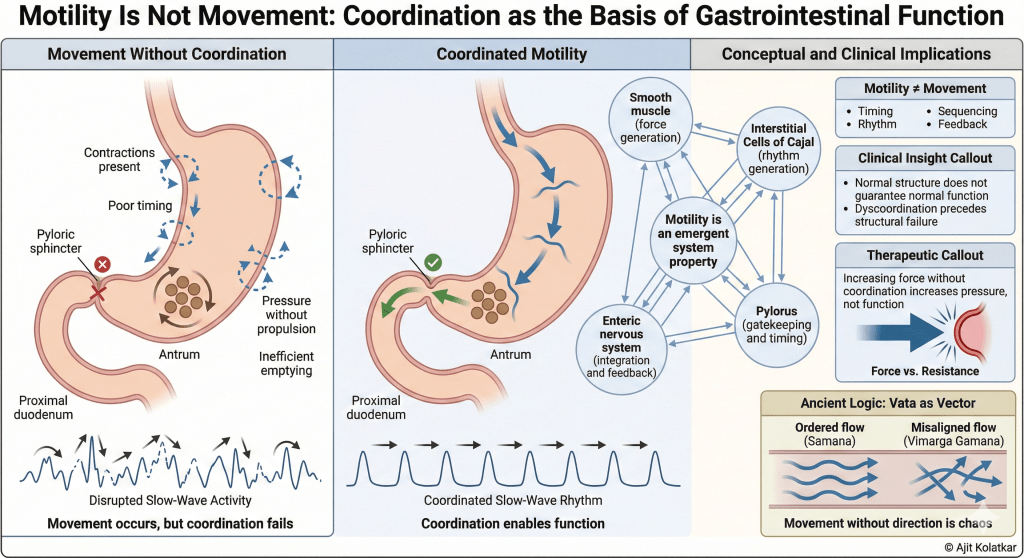
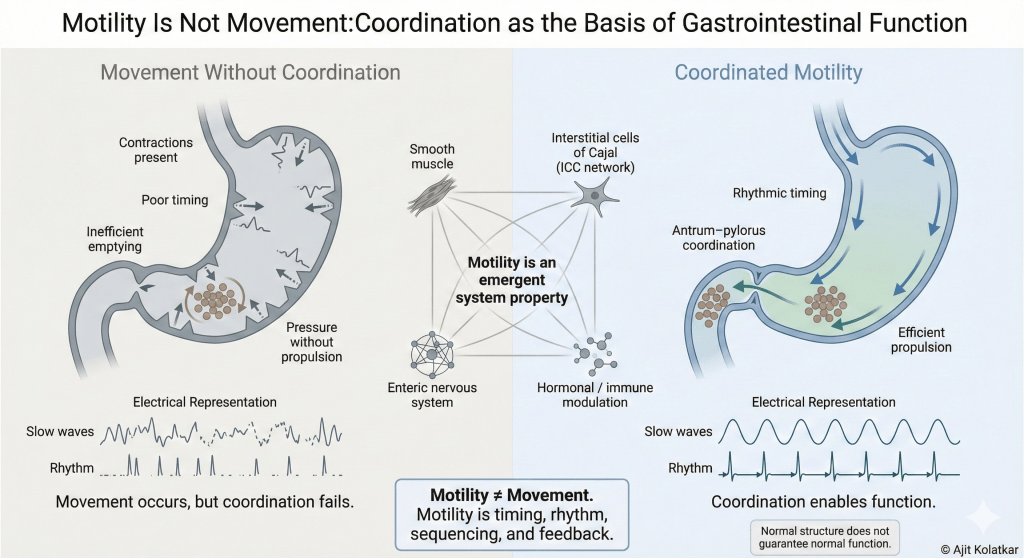
Movement Can Occur Without Coordination
A stomach can move yet still not function.
Contractions may be present but poorly timed while slow waves may propagate yet fail to coordinate with pyloric opening. Intragastric pressure may rise yet empty inefficiently. Basically the gut may appear to be active while being functionally ineffective.
Patients experience fullness, early satiety, nausea, bloating, or pain. Investigations report “normal activity,”imaging reassures and the problem is framed as subtle or functional.
What we observe is that, the movement is there but the coordination has failed.
Motility Is an Emergent Property
Motility is not generated by a single structure. It emerges from interaction.
- Smooth muscle provides the force.
- Interstitial Cells of Cajal generate the rhythm.
- Enteric neurons integrate sensory input and motor output.
- The pylorus acts as a gatekeeper, determining timing and resistance to flow.
None of these components function in isolation. Timing matters more than strength, and sequencing matters more than frequency.
At the cellular level, this coordination is governed by calcium transient clusters (CTC’s). These calcium signals fire at a characteristic frequency that is intrinsic to the Interstitial Cells of Cajal located within the myenteric plexus, a property not shared by other ICC subtypes. This rhythmic signalling entrains smooth muscle contraction and allows spatial and temporal organisation of motility.
What emerges is not simple movement, but pattern.
Like a symphony, individual instruments may continue to play, but without a conductor and shared timing, coherence is lost. It is like the sound persists, but music disappears.
Motility, in this sense, is a system behaviour rather than a mechanical one. It is not just pumping it is……… orchestration.
The Blind Spot of Structural Testing
Structural tests are designed to detect damage, not dysrhythmia.
Endoscopy evaluates mucosa while imaging assesses anatomy and biopsies help detect inflammation or atrophy. These tools excel at identifying lesions, but they are poorly suited to detecting dyscoordination.
A stomach with intact mucosa and normal anatomy can still be profoundly dysfunctional if the electrical architecture is silent or chaotic. Neural signalling may be altered. Pacemaker activity may be unstable.
Structure reassures, but function remains unmeasured.
This gap explains why many patients are told that “nothing is wrong” even when their symptoms clearly suggest that the traffic control system has collapsed.
Interstitial Cells of Cajal: The Conductors
We often describe Interstitial Cells of Cajal (ICCs) as pacemakers, but this description seems incomplete……they are integrators.
They coordinate electrical slow waves. They couple electrical activity to physical contraction while maintaining the spatial organisation of motility patterns.
When these cells dysfunction; a state increasingly recognised as Cajalopathy which does not necessarily abolish movement. It disrupts the symphony. The stomach continues to contract, but the rhythm is lost.
Symptoms emerge not because nothing is happening, but because what is happening no longer works together.
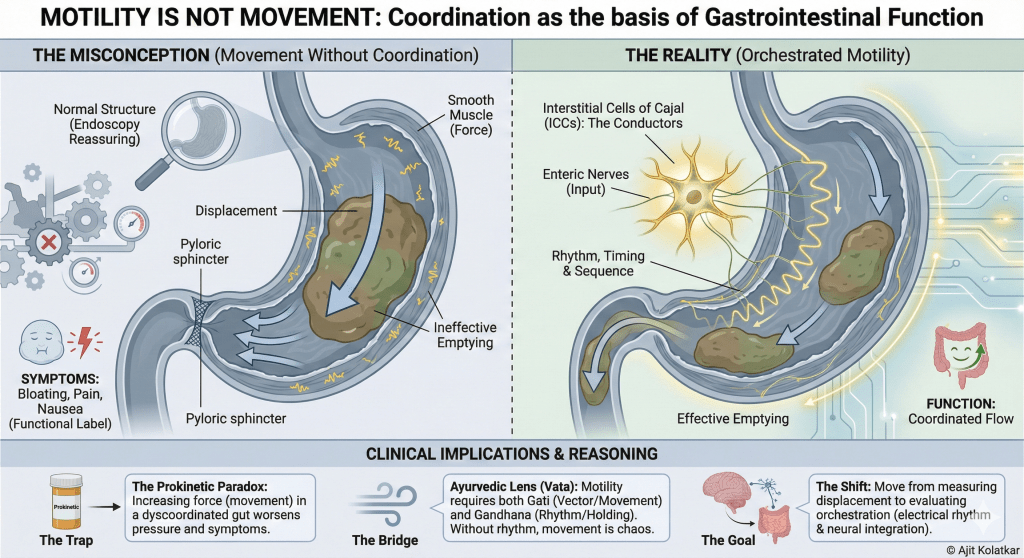
The “Prokinetic Paradox”
If we believe motility is just movement, our treatments remain superficial.
We prescribe prokinetics to “speed things up.” We use acid suppression to treat “reflux.”
But if the problem is dyscoordination, speeding up the transit is like pushing a man who is stumbling. It does not help him walk; it just makes him fall faster.
If the pylorus is not opening in sync with the antral contraction, increasing the force of the contraction only increases the intragastric pressure. The patient feels worse, not better.
Ancient Logic: Vata as Vector
This distinction between movement and coordination is not new. It is central to Ayurvedic reasoning.
In Ayurveda, Vata is often loosely translated simply as “wind” or “air,” (which is a wrong way to think) but in a clinical context, it represents propulsion and direction.
Ayurveda distinguishes between Gati (movement) and Gandhana (the holding or coordination of that movement). When Vata is aggravated, we often see Vimarga Gamana i.e. a movement in the wrong direction or without the correct channel.
The Ayurvedic approach to dysmotility is rarely about just “pushing” the flow (Anulomana). It is about restoring the rhythm (Samana). It acknowledges that movement without direction is chaos.
Why “Functional” Is a Misnomer
When structure is normal and tests are inconclusive, symptoms are labelled “functional.” This label is often intended to reassure, but it frequently invalidates. “Functional” does not mean imaginary, it means that the dysfunction lies at the level of coordination, regulation, and integration rather than anatomy.
Without tools and frameworks to evaluate coordination, “functional” becomes a placeholder for what we cannot yet measure.
A Necessary Reframing
Motility disorders are not disorders of absence but disorders of misalignment.
The gut does not stop working, it works out of sync. Recognising this requires moving beyond visible movement and toward invisible coordination. It requires accepting that normal structure does not guarantee normal function.
Most importantly, it requires listening carefully to symptoms that signal dyscoordination long before structure fails.
Looking Ahead
In the earlier essay, we examined H. pylori as more than an infection, and as a signal of deeper physiological disruption rather than a simple eradication problem.
The next step in this reasoning is to look beyond the stomach and ask what happens when loss of coordination begins to affect downstream regulatory systems.
When motility loses rhythm and timing, consequences rarely remain local. Altered gastric emptying and pyloric coordination reshape bile delivery, enterohepatic circulation, and intestinal sensing. Symptoms migrate, dyspepsia gives way to bowel disturbance. What began as a gastric problem becomes a systemic one.
The next post will explore bile acids not as detergents, but as regulatory signals, and why disturbances in their circulation often explain persistent, shifting symptoms even when infection has been treated and structural tests remain normal.
Motility is not just movement; it is coordination in time and space. When coordination fails, its effects propagate far beyond the stomach.
Leave a comment